Hydrocephalus
General Information, Symptoms, and Treatment
THE INFORMATION PROVIDED BELOW IS GENERAL AND DOES NOT APPLY TO EVERY PATIENT WITH HYDROCEPHALUS. YOU SHOULD GET THE MOST ACCURATE INFORMATION FROM THE NEUROSURGERY SPECIALIST RESPONSIBLE FOR YOUR TREATMENT.
What is Hydrocephalus?
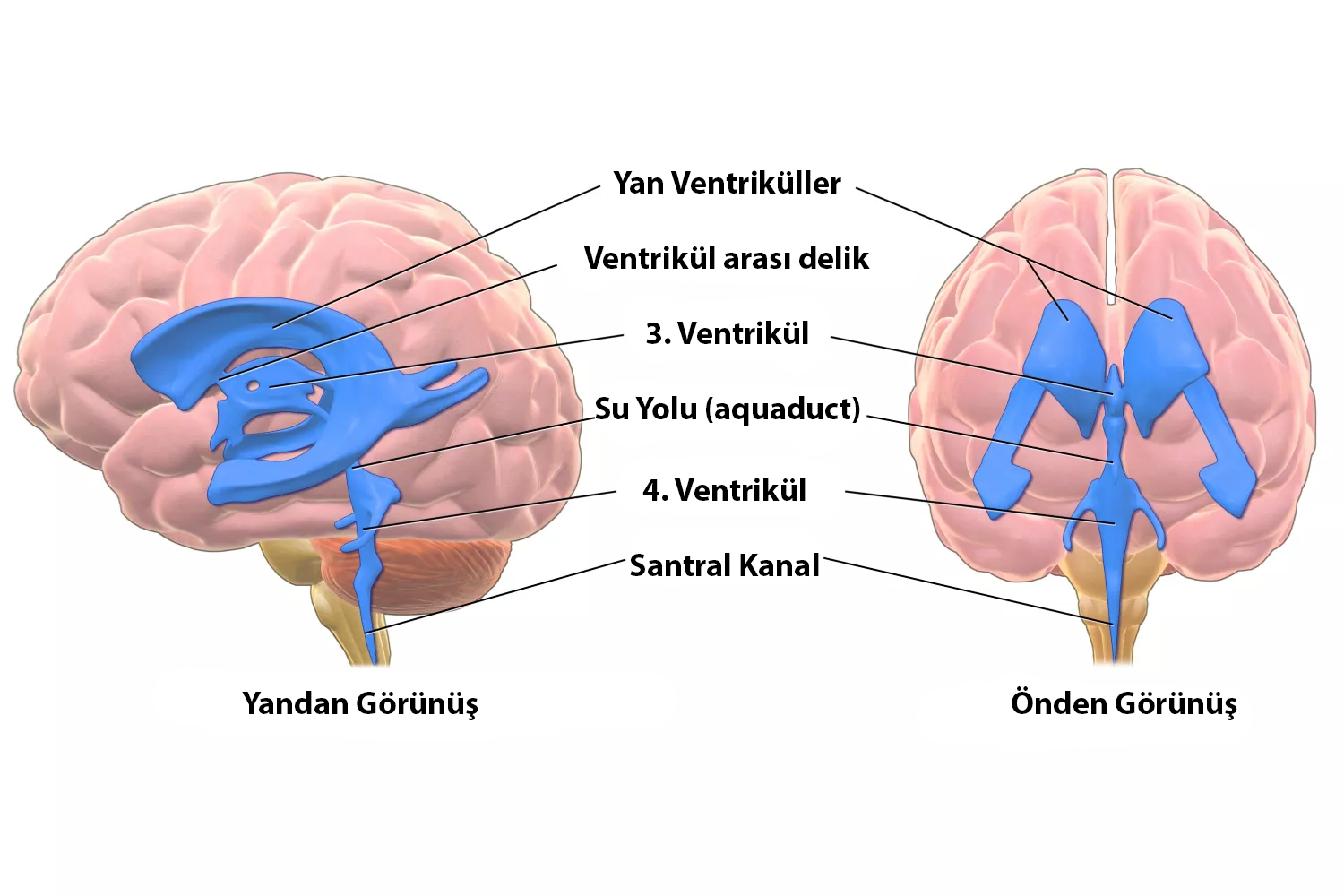
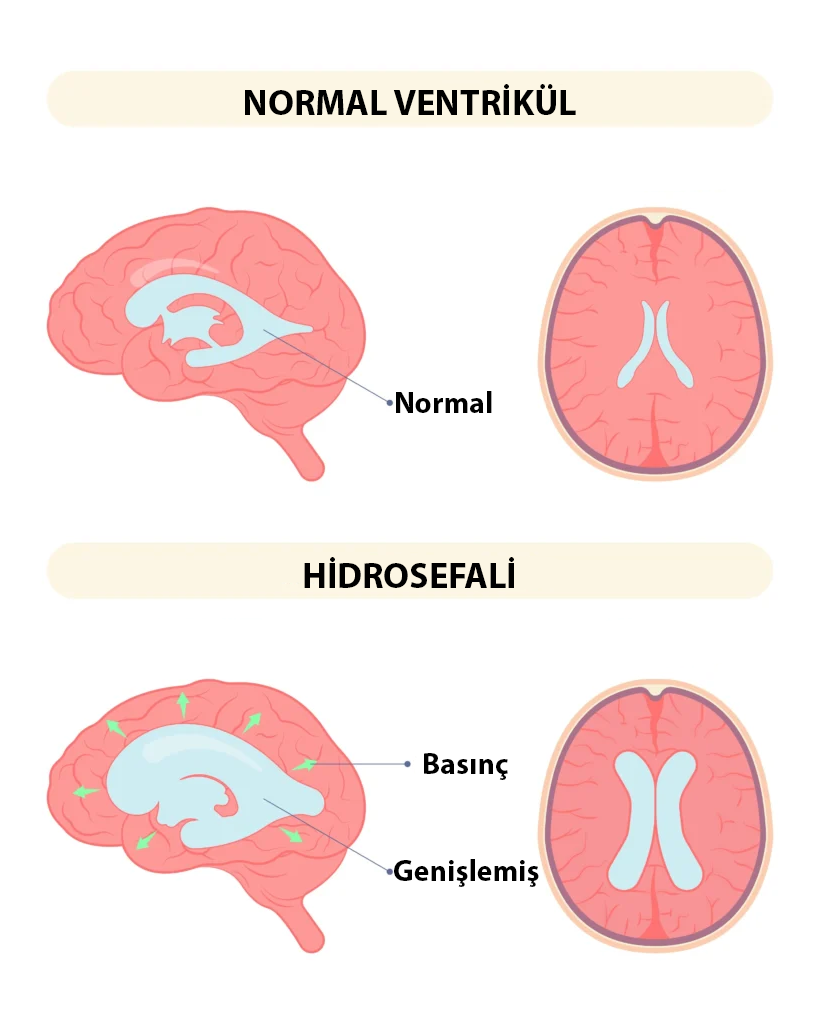
There are cavities, chambers filled with cerebrospinal fluid in every person's brain (these chambers are called ventricles). These cavities are interconnected by thin channels and cerebrospinal fluid continuously circulates between these chambers. The fluid is constantly produced and absorbed by special cells, maintaining a balance in its amount. In conditions where there is an obstruction in the pathways of fluid circulation, impaired absorption of the fluid, or rarely, an increase in fluid production, excess fluid accumulates in these chambers, a condition known medically as HYDROCEPHALUS.
Patients may exhibit the following symptoms:
- Excessive head growth in young children (macrocephaly)
- Nausea and vomiting
- Downward gaze of the eyes - Setting Sun Sign
- Restlessness - Feeding difficulties
- Developmental delays
- Excessive sleepiness
- Seizures (epilepsy)
- Frequent headaches in older children and adults
What Causes Hydrocephalus?
Any problem that affects the circulation of fluid inside the brain can cause hydrocephalus. In some cases, the baby may develop this disease in the womb, while in other cases it may occur due to problems arising later in life.
The main causes of hydrocephalus are:
- Brain hemorrhage due to premature birth
- Brain hemorrhages due to head trauma
- Infections affecting the brain and central nervous system
- Tumors causing excessive cerebrospinal fluid production
- Brain tumors blocking cerebrospinal fluid circulation pathways
- Certain genetic diseases and syndromes
- Developmental anomalies, especially myelomeningocele
.
Is Hydrocephalus a Serious Disease?
When hydrocephalus develops suddenly, it can cause very serious problems and, if left untreated, can even be fatal.
It should be noted that this fatal situation is rare. Since hydrocephalus usually develops slowly, the brain can adapt to this condition and somewhat cope with it. Therefore, if you or a loved one is diagnosed with hydrocephalus, there is often no need to panic. You should consult a neurosurgery specialist as soon as possible.
The way problems associated with hydrocephalus manifest is significantly influenced by the patient's age. In children under one year of age, hydrocephalus may sometimes cause no issues other than rapid head growth. This is because the joints between the skull bones have not yet closed, allowing the increased fluid to enlarge the head circumference and prevent the brain from being compressed and under pressure. Older children and adult patients lack this protective mechanism.
How is Hydrocephalus Diagnosed?
The diagnosis of hydrocephalus starts with suspicion. Especially in small infants, tracking head circumference is one of the most important tools, and consistently more than expected head growth in the following months is the most significant factor raising suspicion. In adults, clinical findings and the patient's complaints typically alert the neurosurgeon to the possibility of hydrocephalus. As mentioned above, because this disease can arise from many different causes, radiological imaging is essential to see why and how the brain is affected. In most cases, the preferred imaging method is magnetic resonance imaging (MRI).
As mentioned above, because this disease can arise from many different causes, radiological imaging is essential to see why and how the brain is affected. In most cases, the preferred imaging method is magnetic resonance imaging (MRI).
Is There a Treatment for Hydrocephalus? What Are the Options?
When hydrocephalus is diagnosed, there are usually very few options other than surgical intervention for treatment. If an identifiable mass is blocking the flow of cerebrospinal fluid (CSF), removing this mass and restoring normal flow can resolve hydrocephalus. However, in most cases, the blockage cannot be removed, and surgical intervention is required to redirect the fluid.
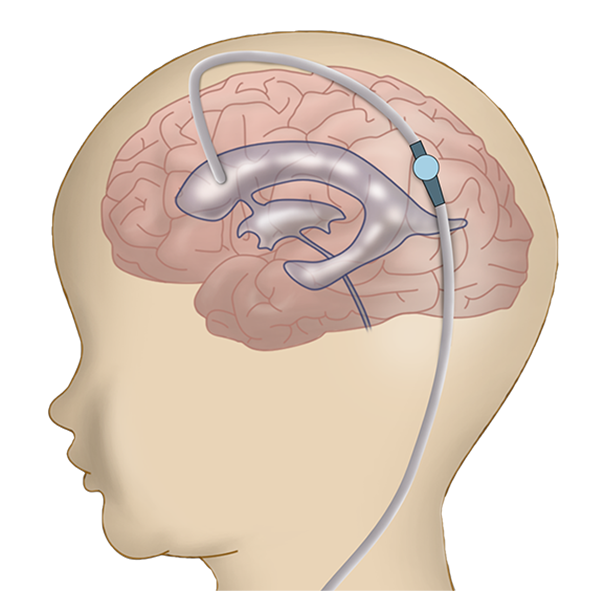
Shunt Systems
The primary goal of hydrocephalus treatment is to redirect the excess fluid accumulated in the brain to another part of the body to prevent it from compressing and damaging the brain. Although it dates back much earlier, the most effective solution found for this problem has been shunt systems, primarily since the 1950s. Medical devices called shunts take the excess fluid from the brain cavity and redirect it to another body cavity through a series of tubes and valves (think of them like faucets) for absorption. The abdominal cavity is the most common destination, but they can also be placed in the heart or pleura.
The most significant advantage of shunt surgery is that it can be applied to EVERY TYPE OF HYDROCEPHALUS and is one of the first surgeries learned by almost every neurosurgeon, making it possible to perform in almost every hospital.
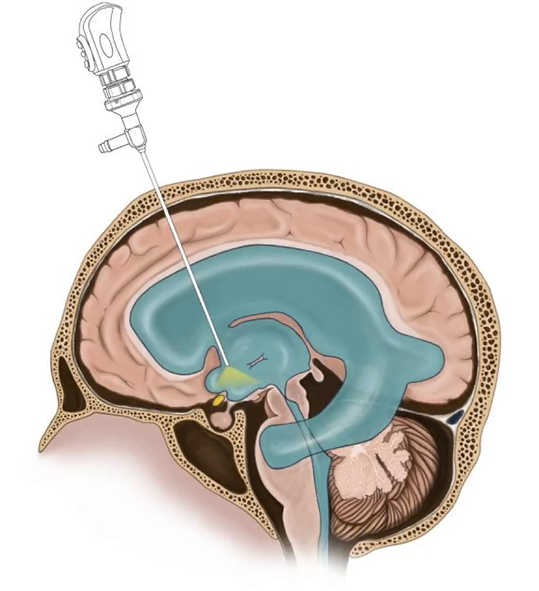
Endoscopic Third Ventriculostomy
In this relatively newer technique, another pathway is roughly created to bypass the obstructed fluid pathways within the brain. Cameras called endoscopes are inserted into one of the brain's chambers, and a hole is made at a suitable location to allow the accumulated fluid to drain and be absorbed from there.
The most important feature is that it does not require the placement of a foreign object into the body as in shunt surgery. It aims to solve the problem entirely with physiological methods within the body.
The most significant disadvantage is that it is NOT SUITABLE FOR EVERY TYPE OF HYDROCEPHALUS. Not every hydrocephalus that can be resolved with a shunt can be resolved with endoscopic methods. There are very clear criteria for patient selection. For example, it is not recommended for infants under one year of age, those with a history of meningitis or brain hemorrhage, or those who have previously undergone shunt surgery. The success rate is significantly lower in such cases. It is most effective when there is a tumor or congenital anomaly, and the fluid pathways are visibly obstructed on MRI. In these patients, the success rate can reach up to 90%.
Another major issue is that it CANNOT BE PERFORMED IN EVERY HOSPITAL by every neurosurgeon. The procedure requires high-tech, quite expensive surgical instruments. Additionally, the surgeon must be trained in this specific technique.
Shunt Surgery
Endoscopic Third Ventriculostomy
Are Hydrocephalus Surgeries Successful?
Before shunt systems were developed into their current forms in the 1950s, hydrocephalus was a highly fatal disease. In the history of medicine, there are very few treatment methods that have directly impacted and made a significant difference in human life as much as shunt systems and shunt surgery.
However, it should be remembered that shunt surgery, like all surgical methods, is not a perfect procedure and is not always 100% successful.
Many factors, including the patient's age and underlying causes, affect the success of shunt surgery. One of the most significant problems with shunts is that they can unfortunately become non-functional. Shunts consist of very small tubes and valves. They can become blocked, break, or, as is often encountered, become infected. Therefore, shunt patients may need to undergo multiple surgeries. This issue is a global problem. Patients operated on in America, Japan, or Turkey all face this issue. The likelihood of a shunt malfunctioning is highest within the first year and relatively decreases over time.
These explanations should not be interpreted as shunt surgery being an unsuccessful surgical procedure. SHUNT SAVES LIVES. The possibility of issues arising exists with every intervention, and the important thing is to deal with these issues correctly when they occur.
Frequently Asked Questions
First of all, I must say that there is no such thing as "easy surgery" and every surgery is equally important to us. However, both shunt surgery and endoscopic surgery are relatively short and low-risk compared to other neurosurgical interventions. Nevertheless, as with any surgery, there are various complication risks, and your doctor will inform you about these.
Both types of surgeries have their own advantages and disadvantages. In cases where both can be applied, the endoscopic method is more physiological and has a lower potential for complications compared to shunt surgery. However, it should be noted that the endoscopic procedure CANNOT ALWAYS BE APPLIED.
These surgeries are not very major compared to many other neurosurgical interventions. The wounds are quite small, and the surgery durations are short. Children and adults tolerate these procedures very well.