Gamma Knife Radiosurgery
Video demonstrates how Gamma Knife Radiosurgery is performed
Gamma Knife Radiosurgery
Gamma Knife Radiosurgery was invented by a Swedish scientist, Lars Leksell. First patient was treated in 1968. 1997 was the first year when the technique was used in Turkey. The device is manufactured by Elekta. Gazi University has installed Gamma Knife device on 2005 and since then has treated over 10 000 patients successfully. Gazi University Department of Neurosurgery has the Gamma Knife Perfexion Model in use.
Although it is not a real knife, neurosurgeons consider Gamma Knife as a surgical tool which uses gamma rays as a scalpel. It targets intracranial pathologies with great precision with the help of its advanced and sophisticated technology. As in real surgery, Gamma Knife targets intracranial pathology and tries to destroy it. Unlike surgery, it has no bleeding, wound and infection complications. Gamma rays sourcing from radioactive Cobalt sources are focused on the target, sparing the normal tissues. A Gamma Knife procedure treats brain lesions with enough radiation to control them, so that they disappear, shrink or stop growing. It can be used to treat targets even in the most critical, difficult-to-access areas of the brain without delivering significant radiation doses to healthy normal brain tissue. It protects normal brain tissue and only targets the diseased tissue. The procedure is performed on an outpatient basis, meaning you will get your treatment approximately in 8 hours and go to your home after this. Patients can return to work and daily activities the next day.

Leksell Stereotactic Frame should be installed to the patient’s head for mapping the brain and the pathology. This is performed under local anesthesia. For patients younger than 10 yo anesthetic sedation is utilized.
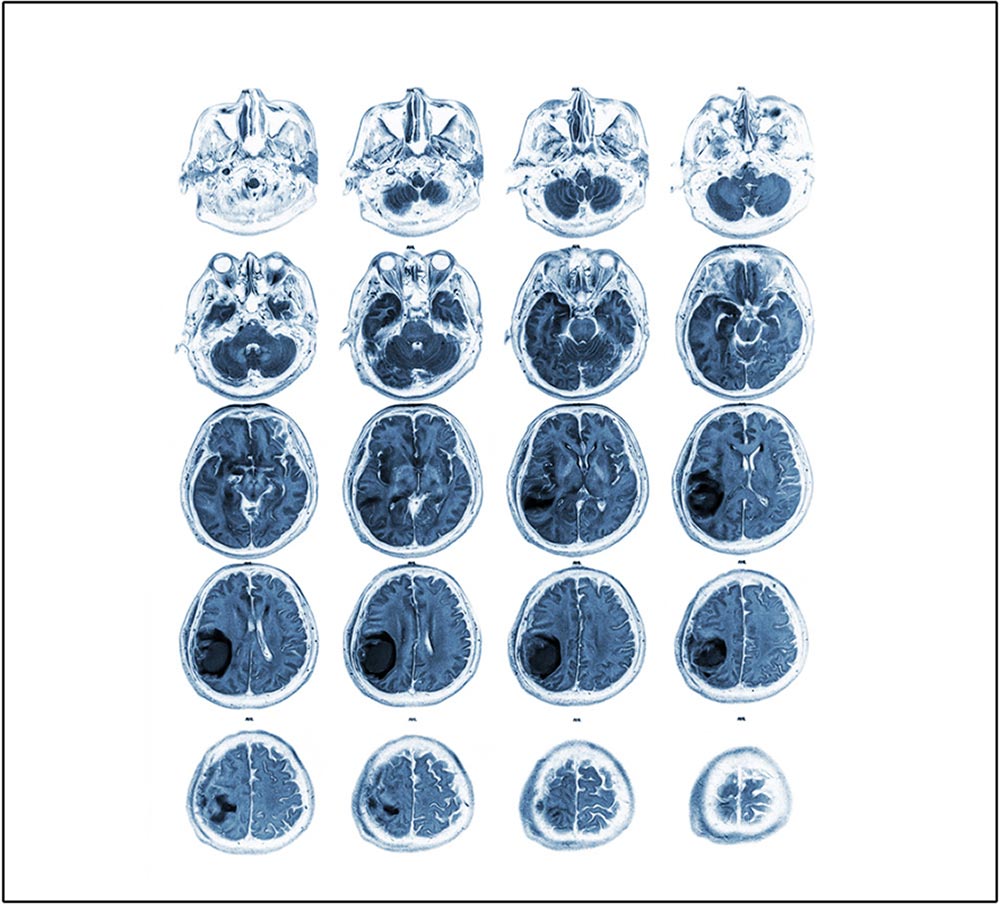
After application of the frame radiologic imaging appropriate for the patient is performed. In all patients, we use MR images. For vascular pathologies, we also add angiography.
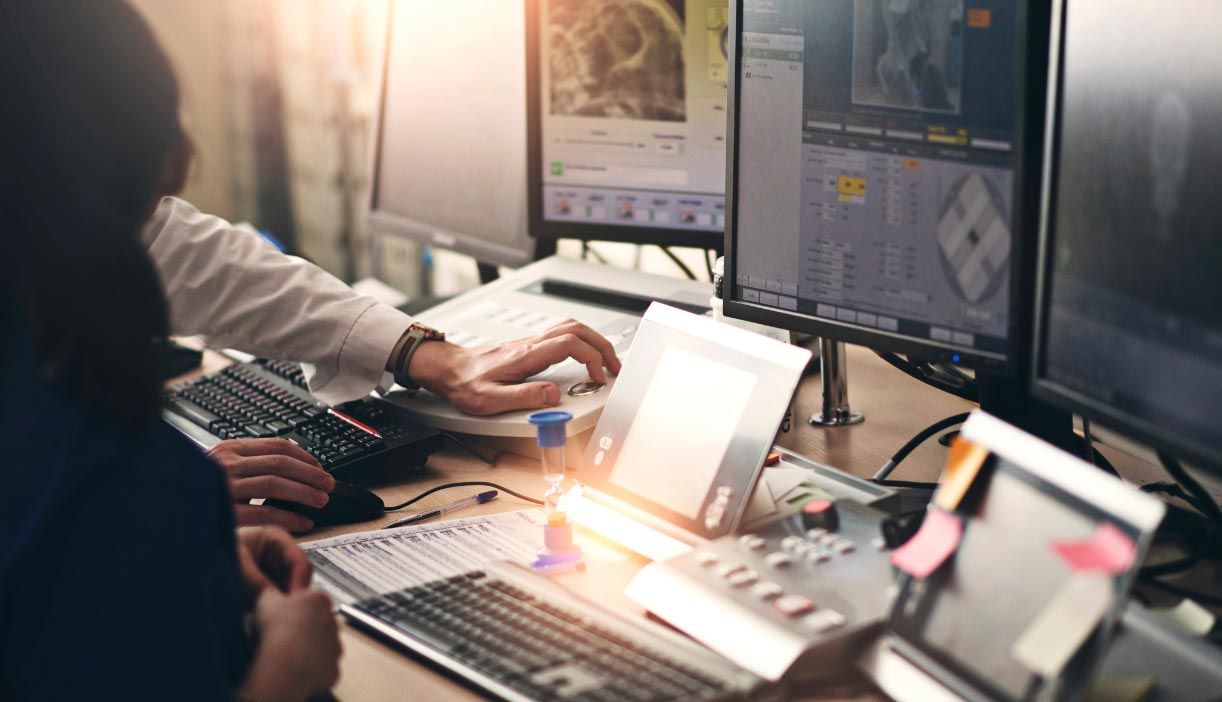
With the help of special computer software called Gamma Plan, the target tissue to be treated is determined with sharp precision and the radiation dose to be applied is determined. In tumors adjacent to sensitive structures, the application of “plugging” can prevent the rays from reaching those critical structures. During these procedures, the patient can spend time chatting and watching TV in his bed.

Once planning is complete, the patient is moved to the treatment room that houses the Gamma Unit. The patient is placed on a couch and positioned into the collimator helmet. The total length of treatment is related to the size and location of the lesion.
I could not understand very well.
Can you explain the procedure?
Gamma knife is a highly evolved and technical RADIATION treatment. Its main characteristic is that it can target the pathological tissue while protecting the normal brain. With this, the side effects of the procedure are extremely rare. High-dose radiation is focused precisely on the pathology with the help of robotic and software technologies. This is its major advantage compared to other radiation therapy modalities. Additionally, since Gamma Knife can only be used for brain pathologies, there is enormous knowledge on the procedure and its results which makes it even safer
Gamma Knife IS NOT SUITABLE FOR EVERY BRAIN DISEASE.
There are various indications for Gamma Knife treatment.
Brain tumors, intracranial vascular anomalies, some
disease-related pain syndromes are among those indications.
Gamma Knife indications are well documented and consist of a
relatively small list. However, with the help of
developments in medicine and technology, new indications are
appearing day by day. Besides the type of pathology, another
important factor in deciding the treatment is the size of
the targeted lesion. In general, Gamma Knife is considered
more effective and safer if the targeted pathology is
smaller than 3 cm (longest diameter).
Another important factor is the location of the tumor. For
example, a very small tumor that is in close proximity to
the optic apparatus (optic nerve) may not be considered a
good candidate for treatment since radiation used during the
treatment may have destructive effects on the visual
pathways. In such a situation, your doctor can offer open
surgery.
The number of peer-reviewed, published scientific articles documenting patient outcomes with Gamma Knife far outweighs any other form of stereotactic radiosurgery. Gamma Knife centers and universities have published more than 2,500 papers and have treated more than 850,000 patients worldwide during the last 40 years. The fact that 75% of all published radiosurgical literature including most of the multicenter trials is based on the use of the Gamma Knife is especially significant given that both Gamma Knife and Linac systems were introduced in the same era.
Gamma Knife is used in over 70,000 patients each year.
Gamma Knife is a neurosurgical tool and it is designed for intracranial pathologies. With the help of recent improvements, we can treat lesions located as low as the level of the second cervical vertebra (most upper part of your neck) however, using Gamma Knife, let’s say, for a lung or liver pathology is impossible.
As with any medical procedure, some risks are involved. Possible delayed complications (6 months or longer) include injury to the surrounding brain and edema, which is reversible with proper treatment. Immediate side effects are extremely rare. The risks of traditional brain surgery, such as hemorrhage, infection, and stroke, are avoided with Gamma Knife radiosurgery.
Gamma Knife treatment itself does not cause pain. For the treatment to be done, a special frame must be fixed to your skull at four points. This is done by numbing the scalp with powerful anesthetic substances, and no pain is felt any more other than this procedure. Since it is not expected for children to be able to adapt this frame procedure, general anesthesia may be performed when necessary for them to alleviate discomfort.
The most important advantage of Gamma Knife therapy is that the treatment can be performed on an outpatient basis. After you come to the clinic in the morning and your procedures are done, you can have your treatment and return home in the evening. In patients requiring general anesthesia, these procedures are usually performed by hospitalizing the patient for one day for safety purposes.
Gamma Knife treatment is a successful treatment method
applied over the world for more than 50 years, but it is not
a magic wand as can be predicted.
For each type of pathology, there is a percentage of success
that is anticipated over the years. For example, Gamma Knife
treatment is considered successful when the brain tumor
stops growing. Gamma Knife will probably not destroy your
tumor or make it disappear. Stopping the growth of the brain
tumor or reducing its size will mean that the treatment is
successful. However, since the physiology and treatment
responses of each body are different and each pathology has
its own characteristics, growth may not be able to be
stopped in rare cases. In such cases, other treatment
options will come into consideration.
On the other hand, the expected result in pathologies such
as arteriovenous malformation (AVM) is to complete the
obliteration of abnormal vessels. Gamma Knife is successful
in this issue by around 70-80%. Within three years, the
vessels that do not occlude completely could be treated with
another session of Gamma Knife or other methods
After the treatment session is finished, the head frame is removed. Sometimes there is a little bleeding from where the pins contact the patient’s head. Gentle pressure is applied to stop the bleeding and some gauzing may be used to keep the pin sites clean. It is usually recommended that the patient refrain from physical activity over the next 18 to 24 hours
Gamma knife treatment is a kind of radiotherapy. The effects of radiation are not immediately apparent. For example, it can take 2-3 years for an arteriovenous malformation to close. Therefore, your collaboration with your neurosurgeon is not over after your treatment. Likewise possible side effects – if they develop – may arise over time rather than immediately after treatment, so you have to come to your regular followups and be under the care of your doctor.